Dr. Wajid Mahmood Khan, Pain Fellow, St Vincent’s University Hospital, Dublin, and Dr Basabjit Das, Consultant in Pain Medicine, St James’s Hospital, Dublin, address the pharmacological management of mild-to-moderate chronic pain
Chronic pain has been recognised as pain that persists past normal healing time, therefore lacking the acute warning function of physiological nociception.
Usually pain is regarded as chronic when it lasts or recurs for more than three to six months. Chronic pain is a frequent condition, affecting an estimated 20 per cent of people worldwide and accounting for 15 per cent to 20 per cent of physician visits. It should receive greater attention as a global health priority because adequate pain treatment is a human right, and it is the duty of any healthcare system to provide it.
Before a physician can treat pain, it is of utmost importance to know the cause of and its severity so a proper plan can be initiated.
Classification of pain
A. Based on pathophysiology:
1. Nociceptive
2. Neuropathic
3. Mixed
B. Based on aetiology:
1. Chronic primary pain not otherwise specific
• Fibromyalgia
• Non-specific lower back pain (LBP)
• Functional abdominal pain syndrome (FAPS)
• Atypical facial pain
2. Chronic cancer pain
• Primary cancer and met-
astases
• Chemotherapy-induced pain
• Pain due to cancer surgery
• Pain due to radiotherapy
3. Peripheral and central nervous dysfunction related
4. Chronic musculoskeletal pain
5. Chronic visceral pain
6. Chronic headache and orofacial pain — primary versus secondary
7. Chronic post-surgical and post-traumatic pain
Pain assessment
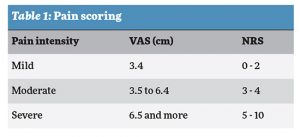
Assessment of pain intensity is considered to be one of the core outcome domains in clinical pain research. Pain intensity is, therefore, widely assessed. Pain intensity is often measured with a self-report single-item measure such as a visual analogue scale (VAS), numeric rating scale (NRS), or verbal rating scale (VRS) (Table 1). The advantage of VRS is that ‘mild’, ‘moderate’, and ‘severe’ are categories often used in communications between patient and healthcare provider in clinical practice.
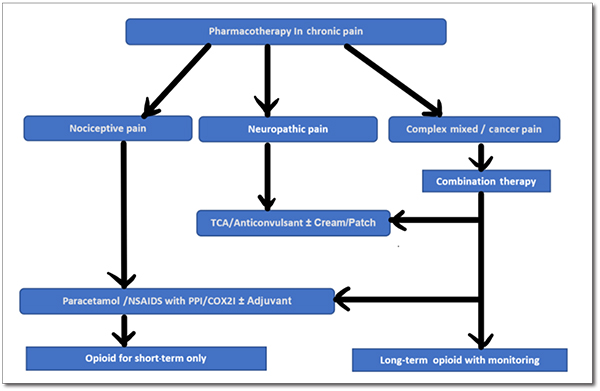
Pharmacotherapy
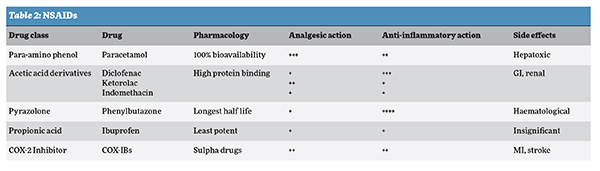
Paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs): The usual approach to treat mild-to-moderate pain is to start with a nonopioid analgesic (Table 2). NSAIDs can be considered in the treatment of patients with chronic nociceptive pain like osteoarthritis.
Cardiovascular and gastrointestinal risks need to be taken into account when prescribing any NSAIDs. Bronchial asthma is not an absolute contraindication and only 25 per cent population is sensitive to it. Paracetamol should always be combined with NSAIDs in the management of pain in such patients. Topical NSAIDs can also be added. COX-2 selective NSAIDs have equivalent efficacy, and a similar range of adverse effects, to those of conventional NSAIDs. Therefore, they are not preferred routinely to conventional NSAIDs. They should only be considered in patients with significant gastrointestinal problems. Extra caution should be practiced when these drugs are given to subjects with pre-existing hypertension, renal disease, and heart failure.
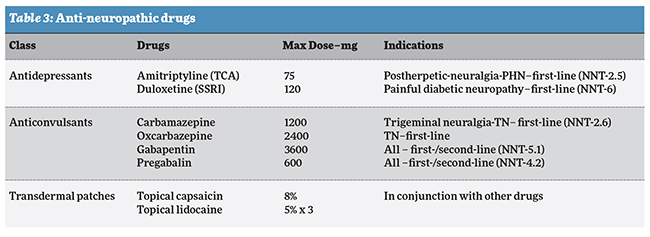
II. Anti-neuropathic drugs: Consideration should be given to vulnerabilities to adverse effects with anti-neuropathic pain medications and comorbidities, lifestyle factors, any mental health problems and interactions with other medications. Monitor the effectiveness of the chosen treatment, assess overall improvement and gradual dose reduction if improvement sustained.
Patients with chronic pain conditions using antidepressants should be reviewed regularly and assessed for ongoing need and to ensure that the benefits outweigh the risks. Tricyclic antidepressants should not be used for the management of pain in patients with chronic low back pain which is solely nociceptive. Amitriptyline could be considered for the treatment of patients with fibromyalgia and also duloxetine.
Carbamazepine should be considered for the treatment of patients with trigeminal neuralgia and facial pain of neuropathic type (Table 3). Potential risks of adverse events of such medication include low blood cell counts and sodium and levels should be regularly monitored. Oxcarbazepine is the safer version which requires no monitoring.
Capsaicin (8%), a transient receptor potential vanilloid (TRPV) receptor antagonist or lignocaine (5%) patches should be considered in the treatment of patients with peripheral neuropathic pain when first-line pharmacological therapies have been ineffective or not tolerated and mostly used in conjunction. Initially capsaicin 0.075 per cent can be used for neuropathic pain, and capsaicin 0.025 per cent for arthritic pain can be tried.
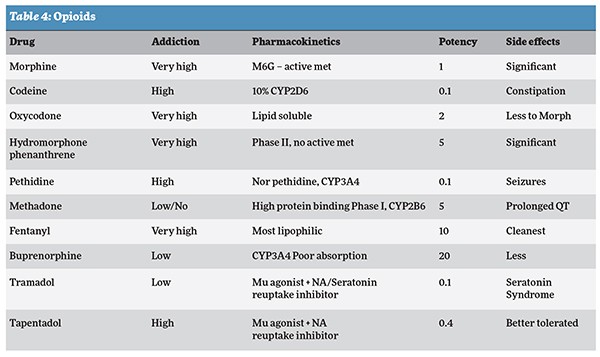
III. Opioids: Mild opioids can be considered in common painful conditions but with cautions. Strong opioids should only be considered as an option for pain relief in patients with cancer pain and chronic nociceptive pain refractory to all other medications and pain interventions and only continued if there is ongoing pain relief (Table 4).
Tramadol or tapentadol can be prescribed for neuropathic pain or mixed type of pain provided there is no contraindication.
Patients started on opioids should be advised of the likelihood of side effects such as nausea, constipation, addiction liability and long-term hormonal effects like osteoporosis. They should be assessed regularly for changes in pain relief, side effects and quality of life, with consideration given to a gradual reduction to the lowest effective dose. There should be careful assessment of pre-existing risk factors for developing opioid misuse.
It is always better to stick to one medication, one route and prescriber. The US Centers for Disease Control and Prevention (CDC) Guidelines (www.cdc.gov) address patient-centred clinical practices including conducting thorough assessments, considering all possible treatments, closely monitoring risks, and safely discontinuing opioids.
The three main focus areas
A. Determining when to initiate or continue opioids for chronic pain:
• Selection of non-pharmacologic therapy, nonopioid pharmacologic therapy, and opioid therapy
• Establishment of treatment goals
• Discussion of risks and benefits of therapy with patients
B. Opioid selection, dosage, duration, follow-up, and discontinuation
C. Assessing risk and addressing harms of opioid use:
• Evaluation of risk factors for opioid-related harms and ways to mitigate patient risk
• Review of prescription drug monitoring program (PDMP) data
• Use of urine drug testing
• Considerations for co-prescribing benzodiazepines
• Arrangement of treatment for opioid use disorder
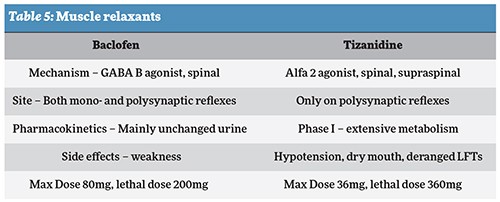
IV. Muscle relaxants: Skeletal muscle relaxants are a broad class of pharmacological agents used for the treatment of muscle spasticity, although many of these agents cause a high degree of side effects including sedation. Most skeletal muscle relaxants are FDA approved for either spasticity (baclofen, tizanidine) or musculoskeletal conditions. They can be used as adjuvant therapy to treat myofascial pain including lower back.
This might help more in an acute and sub-acute state and there is little evidence to support that these drugs become the standard of treatment for chronic pain.
V. Combination therapy: Combination therapies should be considered for patients with complex pain, cancer pain and mixed pain. In patients who do not respond to anti-inflammatory and anti-neuropathic, and who are unable to tolerate other combinations, consideration should be given to the addition of an opioid such as morphine or oxycodone but again with great caution. Polytherapy can allow the use of lower dosages of each individual agent, possibly minimising side effects and risks.
Summary
A number of medications have proven to be effective and their use individually or in combination should improve the management of chronic pain. However, evidence is not strong for most of the medications that we use in chronic pain. Typically, nonopioid analgesics are first-line treatment, including paracetamol, NSAIDs, and topical drugs.
Balancing the consequences of chronic pain and long-term side effects of medications is a serious challenge to achieve a critical goal. Goal of pharmacological pain management may not be a score of zero but patient should be satisfied and functional with no unpleasant side effects of therapy.
Proper diagnosis and assessment remain the cornerstone to choose the most relevant pharmacotherapy. Understanding the risks and benefits of common pain medications can help you make safe choices. Always start with the first-line treatment and consider second-line treatments only in selected clinical circumstances.
A thorough understanding of pain mechanisms and good communication between physicians and patients are required to improve patient outcomes.
Avoiding medications like opioids and maximising effective medications have always been proven beneficial. Because of the potential for serious adverse effects, opioids should be prescribed only if the clinician is familiar with their use and associated risks.
Additionally, identifying and co-managing comorbidities including psychiatric disorders will have a huge impact on pain management.
Furthermore, incorporation of the multi-modality approach with pharmacotherapy will provide the best modality for both pain relief and rehabilitation.
• Wajid Mahmood Khan is a Pain Fellow, St Vincent’s University Hospital, Dublin.
• Dr Basabjit Das is a Consultant in Pain Medicine, St James’s Hospital, Dublin.
This article is also published on the IMT(Irish Medical Times) site click here to read.

